Endometriosis: How it affects every decade of your life
From leaking in class to missed days at work, Molly May reveals what a lifetime of endometriosis is like through four women's stories.
As 18-year-old Chloe Miller sat alone in a hospital gown waiting to be wheeled down to theatre, she felt scared.
As the anaesthetic was injected, her final thoughts were on the potential outcomes of the surgery.
"I was worried that if they didn't find anything, I would go back to being called lazy and people would think I was putting it on.", Chloe says.
Chloe is one in ten women that has been diagnosed with endometriosis, and like many women, she did not expect something as natural as a period to lead her to a life of surgeries.
Endometriosis is a condition where tissue, similar to the lining of the womb, grows elsewhere in the body, such as the ovaries or fallopian tubes.
The cause is unknown and there is currently no cure.
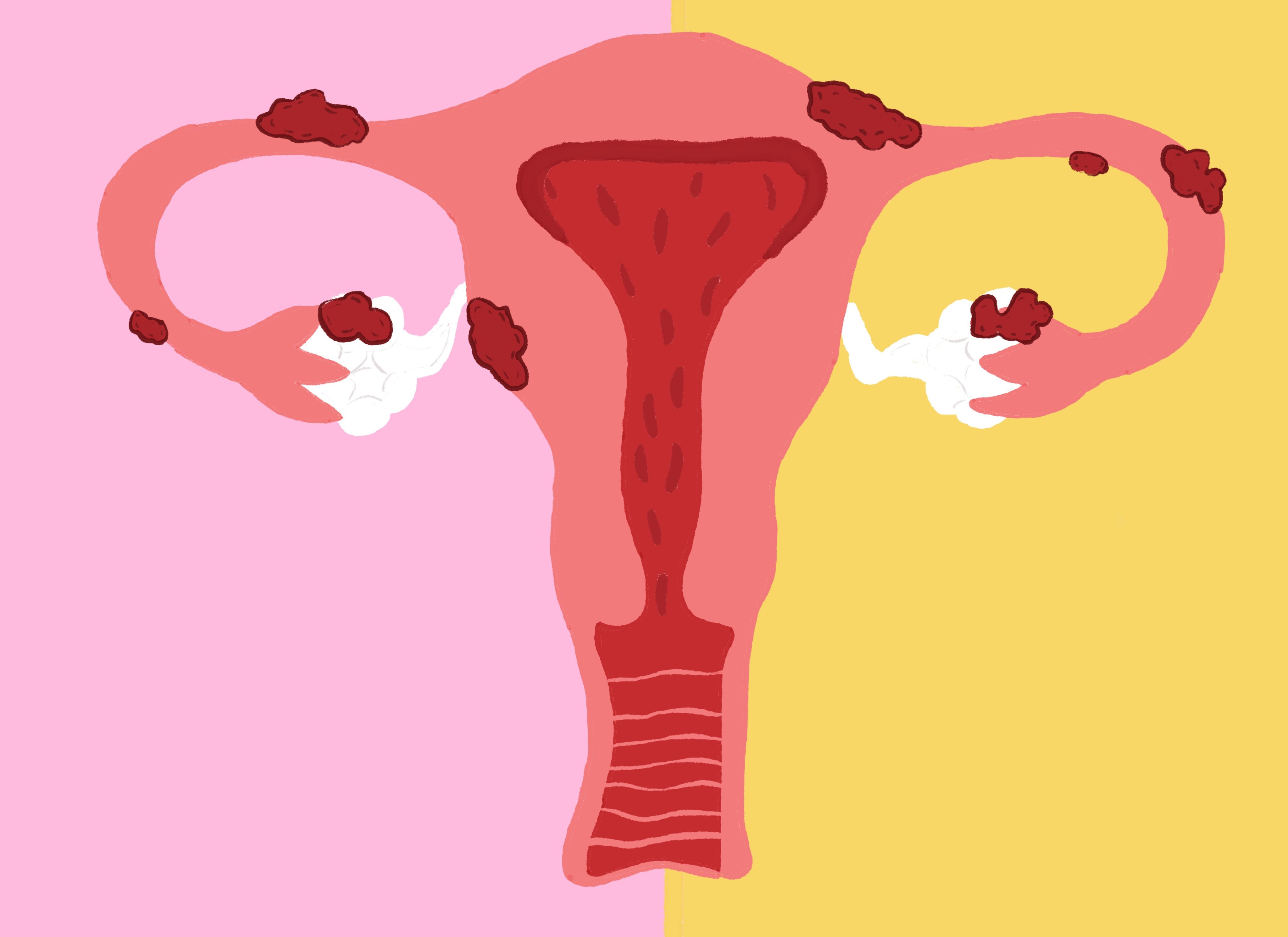
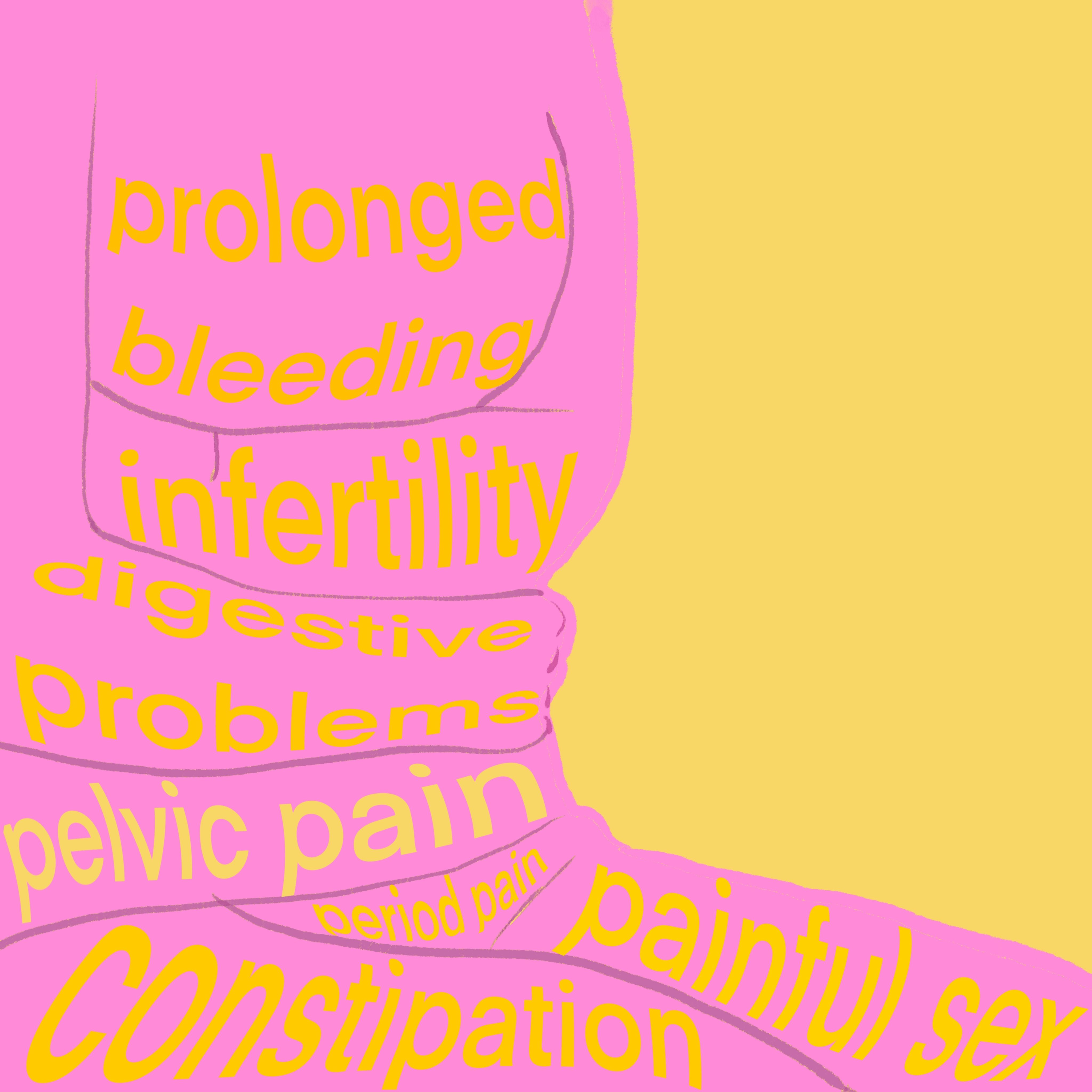
Endometriosis symptoms can include: chronic pain, heavy periods, infertility problems, fatigue, painful sex and much more. Image credit: Harry May
Endometriosis symptoms can include: chronic pain, heavy periods, infertility problems, fatigue, painful sex and much more. Image credit: Harry May
18-year-old Chloe Miller
When Chloe Miller started her first period aged 10, she knew something was wrong.
She suffered heavy and prolonged bleeding with excruciating pain that left her feeling suicidal.
"The pain made me feel like I didn't have a place on this earth," Chloe, from Devon, says.
"Because of everything, I actually had a suicide attempt, so I was in hospital during my GCSEs."
Despite hospital stays, trialling different contraceptive pills, and being misdiagnosed with fibromyalgia and IBS, Chloe underwent laparoscopic surgery in July, 2021, that revealed she had endometriosis.
Chloe explains how her chronic illness devastatingly impacted her school years.
"I actually didn't go to school on my period; they were that bad," Chloe says.
"I had to change my pad every twenty minutes and got denied going to the toilet a lot, so I just didn't go in."
Chloe claims her school was unsupportive and made her feel she was lazy for missing her education.
"I physically couldn't go in because of how much pain I was in," Chloe explains.
"I tried my hardest despite the fact that it's how I felt every day."
Despite her hospitalisation, Chloe passed English and is now training to be a veterinary nurse.

Chloe would often have to go to A&E due to how heavy her periods were. Image credit: Chloe Miller
Chloe would often have to go to A&E due to how heavy her periods were. Image credit: Chloe Miller

Chloe says her pain began to return a few months after surgery and potentially faces future operations. Image credit: Chloe Miller
Chloe says her pain began to return a few months after surgery and potentially faces future operations. Image credit: Chloe Miller
Chloe spent four to five days a month absent from school due to her periods. Image credit: Chloe Miller
Chloe spent four to five days a month absent from school due to her periods. Image credit: Chloe Miller
It took six years to receive a diagnosis and Chloe was told several times by doctors that she was 'too young' to have endometriosis, despite her aunt having the condition.
Chloe feels her age delayed her diagnosis and was never told why she had to wait until the age of 18 to have surgery.
General Practitioner Dr Pav Tandon, at the Cedar Medical Practice in Lincolnshire, explains how ageism is not intentional when considering a diagnosis.
"A 17, 18, 19-year-old with pelvic pain will probably be approached slightly differently from someone who's 35 or 45 because there is more urgency to rule out cancer in those who are older.
"You can't say that there's an age group that be excluded from endometriosis, because it affects all ages, however you're more likely to get diagnosed when you're older due to menstrual retrograde bleeding spilling into the contents of the pelvis, which becomes more embedded as time passes.
"You have to make sure you rule out infection first as infection can present with similar symptoms, before you consider endometriosis.", Dr Tandon explains.
Having battled through her school years, Chloe hopes schools do more to support young people suffering with the condition, something 25-year-old primary school teacher, Shannon Reed, could not agree with more.

Dr Tandon says GPs are now robustly trained in medical school to identify a patient presenting with endometriosis symptoms. Image credit: Dr Pav Tandon
Dr Tandon says GPs are now robustly trained in medical school to identify a patient presenting with endometriosis symptoms. Image credit: Dr Pav Tandon
Dr Tandon says that regardless of age it is important for GPs to consider endometriosis as a diagnosis in women presenting with pelvic pain.
Dr Tandon says that regardless of age it is important for GPs to consider endometriosis as a diagnosis in women presenting with pelvic pain.
25-year-old Shannon Reed
Having also started her periods young, Shannon Reed, from Essex, began to experience extremely painful periods from 15-years-old.
After being hospitalised by pain at 15, 17 and 18-years-old for ovarian cysts, Shannon was diagnosed with endometriosis at age 20.
Shannon describes how her pain controlled her life and left her feeling 'isolated'.
"I remember feeling really isolated from a social perspective because it was hard for friends to understand," Shannon says.
"They could still get up, go out the house, go to the movies, take a couple tablets and be fine, whereas I was in agony and couldn't go anywhere.
"I felt like, mental health wise, I was always going to be the one that no one particularly understands."
After two surgeries and being told she would never be able to have children, Shannon unexpectedly fell pregnant with son Riley.
Shannon explains how her pregnancy was not enjoyable.
"I spent every moment during my pregnancy thinking I was going to lose my child because I had complications - and that was horrific," Shannon emphasises.
"I don't think professionals, to some extent, have enough information because I find myself explaining my condition over and over again."
Shannon says clinical language can also make patients feel isolated and that diagnosis should be explained in terms patients can understand.
She feels her diagnosis was delayed due to a lack of education of the disease among medical professionals and peers and believes women would get diagnosed quicker if they were educated about menstrual health issues from a young age.

Shannon, aged 20, supported by her mum, Francine Reed, in hospital for removal of cysts in 2017. Image credit: Shannon Reed
Shannon, aged 20, supported by her mum, Francine Reed, in hospital for removal of cysts in 2017. Image credit: Shannon Reed

Shannon has now had two surgeries for her endometriosis and continues to manage her pain with medication when required. Image credit: Shannon Reed
Shannon has now had two surgeries for her endometriosis and continues to manage her pain with medication when required. Image credit: Shannon Reed

From left: Shannon Reed with her partner Callum Yates and son Riley. Image credit: Shannon Reed
From left: Shannon Reed with her partner Callum Yates and son Riley. Image credit: Shannon Reed

Shannon says fertility information should be discussed thoroughly with with endometriosis patients to ensure they leave empowered with the knowledge to make future decisions. Shannon pictured with son Riley. Image credit: Shannon Reed
Shannon says fertility information should be discussed thoroughly with with endometriosis patients to ensure they leave empowered with the knowledge to make future decisions. Shannon pictured with son Riley. Image credit: Shannon Reed
Shannon Reed says it is important to include boys in menstrual health discussions from a young age.
Shannon Reed says it is important to include boys in menstrual health discussions from a young age.
Despite the Department for Education making menstrual health compulsory in the national curriculum from September 2020, the Relationships and Sex Education (RSE) statutory guidance does not specify teaching on menstrual issues such as endometriosis.
Shannon says that whilst RSE remains a foundation subject, menstrual health will not be a priority.
"It's a very touchy subject for schools because it's still viewed as too invasive," the primary school teacher says.
"It's not a core subject like English, Maths and Science, and therefore will be neglected to some level and dropped in order for a test paper."
Shannon claims that the quality of teaching for RSE is dependent on the teacher at the front of the classroom.
She adds: "It depends on the teacher's comfort, knowledge and experience.
"I would happily stand in front of my classroom and teach pupils about their bodies, but another teacher may feel uncomfortable about some of the concepts and brush over it."
Medical student Hassan Qadri, from the University of Plymouth, agrees that education among medical professionals remains a top reason for a delayed diagnosis, which can lead to sexist attitudes.
Despite the Royal College of General Practitioners including gynaecology in medical school curriculums, the General Medical Council stated in a report that graduates do not learn complex issues and that "doctors in training are only exposed to women's health issues opportunistically on placement".
"I think there is a lack of understanding and consistency when it comes to women's health and it's one of the biggest issues in terms of recognising the severity of related conditions," Hassan Qadri says.
"The knowledge of medical centres nowadays has got better, but there's always room for improvement.
"Being in a clinical environment really helped me understand the variability of women's health, so I think recognition and appreciation of that, in first and second year, would probably benefit people a lot more in training."
Hassan Qadri says the biggest learning outcome from his gynaecology placement was gaining a better understanding of women's health.
Hassan Qadri says the biggest learning outcome from his gynaecology placement was gaining a better understanding of women's health.
Whilst Shannon pushes endometriosis education, she acknowledges the lack of understanding in the workplace as an adult, something 31-year-old Danni Hopkins is all too familiar with.
31-year-old Danielle Hopkins
Demand planning manager Danni Hopkins, from Surrey, began experiencing painful periods in March, 2021, a few years after coming off the contraceptive pill.
"I honestly felt like I was being stabbed," Danni describes.
"I was in tears.
"It made me throw up.
"I was literally crawling the walls and popping Naproxen like it was candy."
After seeing a GP in June, 2021, who referred her to gynaecology, Danni had a laparoscopy in August the same year which revealed she had severe stage four endometriosis.
Due to it being close to her bowel, Danni learned she would need another surgery to remove the rest.
Danni, who is used to working internationally, explains how her endometriosis impacts her employment.
"I feel like there are a lot less options open to me now," Danni says.
"You've got this thing in the back of your head like 'What if I need a doctor?' or 'What if that's the week of my period and I'm going to be in lots of pain on a buying trip?'.
"I have limits now."
Danni had a two-year contract lined up for working in Qatar but backed out due to the fear of being in pain and needing more procedures.
She adds: "For these procedures, you rely on being picked up by someone and having support, and I wouldn't have anybody.
"Three years ago, I would've jumped the opportunity, whereas now, I feel like until this is totally under control and I'm on a long-term treatment plan, I don't feel comfortable doing those things."

Danni Hopkins says employers need to be more understanding of the condition and that women with endometriosis can feel embarrassed by needing time off work due to pain. Image credit: Danni Hopkins
Danni Hopkins says employers need to be more understanding of the condition and that women with endometriosis can feel embarrassed by needing time off work due to pain. Image credit: Danni Hopkins

From left: mum, Lisa, shares the same condition with her daughter, Danni Hopkins. Image credit: Danni Hopkins
From left: mum, Lisa, shares the same condition with her daughter, Danni Hopkins. Image credit: Danni Hopkins
Danni Hopkins says she felt embarrassed to fill in her work declaration form due to the stigma around non-visible health conditions.
Danni Hopkins says she felt embarrassed to fill in her work declaration form due to the stigma around non-visible health conditions.
The APPG on Endometriosis inquiry report found that 55 per cent of women took time off work, 38 per cent feared losing their jobs, and 35 per cent had a reduced income as a result of the impact of their endometriosis.
Endometriosis UK launched the Endometriosis Friendly Employer Scheme in 2020 to help develop a supportive work environment for employees living with the disease.
Endometriosis UK volunteer and South Essex support group founder, Sarah Smallbone, works alongside the National Institute for Health and Care Excellence (NICE) to improve endometriosis guidelines.
She faced disciplinaries at work for exceeding average sickness with her endometriosis despite having worked at her employment for over six years.
Sarah says that endometriosis is a "massive economy problem" and hopes the scheme encourages women to have conversations with employers that have more understanding of the disease.
"I think there is still a lot of stigma attached to talking about it in the workplace, and I think it will take a while to change, especially with more males in management roles - thought not to say that all women understand it either," Sarah Smallbone says.
"It starts with education and until menstrual health is made a normal conversation in schools, there will be an element of pushback.
"By the time women get to the workplace, there is already a stigma there."

Sarah Smallbone says women's health should not be a taboo in the workplace and encourages employers to join the scheme to support those with the condition. Image credit: Sarah Smallbone
Sarah Smallbone says women's health should not be a taboo in the workplace and encourages employers to join the scheme to support those with the condition. Image credit: Sarah Smallbone

Far right: Sarah Smallbone with other Endometriosis UK representatives at the first APPG on Endometriosis meeting. Image credit: Sarah Smallbnone.
Far right: Sarah Smallbone with other Endometriosis UK representatives at the first APPG on Endometriosis meeting. Image credit: Sarah Smallbnone.

Sarah Smallbone, second from right, helped organise the annual Endo March 2016 event in London. Image credit: Sarah Smallbone
Sarah Smallbone, second from right, helped organise the annual Endo March 2016 event in London. Image credit: Sarah Smallbone

Sarah Smallbone pictured front centre at the annual Endo March 2016. Image credit: Sarah Smallbone
Sarah Smallbone pictured front centre at the annual Endo March 2016. Image credit: Sarah Smallbone
Sarah Smallbone says it is important to teach girls about menstrual abnormalities to give them the knowledge and confidence to seek help.
Sarah Smallbone says it is important to teach girls about menstrual abnormalities to give them the knowledge and confidence to seek help.
MP Christian Wakeford for Bury South says that endometriosis should be recognised as a disability and that government needs to do more to support women in schools and workplaces.
"Women's health isn't taken seriously unless men talk about it - and that's not right," MP Christian Wakeford says.
"Government isn't doing anywhere near enough when there is much more money being spent on men's health, such as erectile dysfunction.
"Women make up over half the population and it's about time they're heard."
Danni worries about the impact her endometriosis will have on later life, which is something her 58-year-old mum, Lisa, says continues.
MP Christian Wakeford for Bury South says at the Endo Support United Conference 2022 that he's saddened by the fact that some women take their own lives due to the pain and urges government to take endometriosis more seriously to provide specialist care.
MP Christian Wakeford for Bury South says at the Endo Support United Conference 2022 that he's saddened by the fact that some women take their own lives due to the pain and urges government to take endometriosis more seriously to provide specialist care.
58-year-old Lisa Hopkins
At 26-years-old, hairdresser Lisa Hopkins, from Surrey, was diagnosed in 1990 with stage one endometriosis after fighting to get a diagnosis for three years.
"It felt like my fallopian tubes were burning and I had a constant dragging pain," Lisa, mother of Danni, says.
"The only way I can describe it was like my fallopian tubes had heartburn."
One of the problems Lisa faced getting a diagnosis was being believed by her doctors, who after multiple tests and appointments, told her to see a specialist privately.
Lisa says she felt "elated" to get a diagnosis after being made to feel "crazy" by her doctors for years, who had never suggested endometriosis.
Lisa explains: "That was like joy, because I thought, well at least I'm being believed.
"At least someone thinks there's something wrong with me because I know my body and I know something is wrong."
Lisa spent most of her adult life in pain and tried various treatments to ease her symptoms including taking the contraceptive pill.
Her constant dragging pain caused her to have two surgeries to remove her endometriosis and eventually a hysterectomy at age 51, though this procedure is not necessarily a treatment.
Lisa explains how her endometriosis impacted her her work and family life, with pressures on having children.
"I was told there was a chance that I may not have children," Lisa says.
"I had just bought my own business at the time and wasn't really thinking about children yet, but I was told if I was going to have children, then I needed to have them now.
"It feels like you have to have children when they tell you to and something that can be forced on you when you're not even ready."
Lisa says endometriosis affects every stage of your life and says women's health issues are not recognised enough.
"There's always a next step," Lisa explains.
"The diagnosis is one hurdle you get over because you're believed, and then if you want children, you've got to rush that, and then another laser treatment.
"No matter what point you're at, it just doesn't stop."
Now aged 58, menopause has significantly reduced Lisa's pain and she is looking forward to getting back in the gym.

From left: Lisa Hopkins, pictured with daughter Danni, says endometriosis impacts every stage of a woman's life including having a career and being able to have children. Image credit: Danni Hopkins
From left: Lisa Hopkins, pictured with daughter Danni, says endometriosis impacts every stage of a woman's life including having a career and being able to have children. Image credit: Danni Hopkins

From right: Lisa Hopkins pictured with her mum, Joan Stupple, who had suspected endometriosis but was never diagnosed. Image credit: Danni Hopkins
From right: Lisa Hopkins pictured with her mum, Joan Stupple, who had suspected endometriosis but was never diagnosed. Image credit: Danni Hopkins

Despite fertility warnings from medical professionals, according to Endometriosis UK, it is estimated that 60 to 70 per cent of endometriosis patients can conceive, although there is still a lack of research on how the condition affects fertility. Image credit: Harry May
Despite fertility warnings from medical professionals, according to Endometriosis UK, it is estimated that 60 to 70 per cent of endometriosis patients can conceive, although there is still a lack of research on how the condition affects fertility. Image credit: Harry May
From left: Lisa Hopkins, with daughter Danni, says there is a lot of pressure on women with endometriosis to rush having children.
From left: Lisa Hopkins, with daughter Danni, says there is a lot of pressure on women with endometriosis to rush having children.
Endometriosis specialist and laparoscopic surgeon at The Lister Hospital, Mr Shaheen Khazali, as seen on BBC 2's Your Body Uncovered, says the impact of endometriosis on women's lives can be as devastating as cancer.
"This comment comes from an experience with a patient of mine who told me she wished she had cancer - and that really hit hard for me," Mr Khazali explains.
"When I asked why, she said 'because everyone understands cancer'.
"With endometriosis, her boss says it's just a period, her mother tells her to get on with it, her husband thinks she doesn't love him because she doesn't want to have sex, and no one knows any answers or who's the right specialist.
"It's a benign condition, but it can wreck women's lives the same way cancer can."
Mr Khazali says social media is having a positive effect on the future care of endometriosis patients and that analysing patients' journeys will be the key to moving forward.
"It's really given patients the voice and power to lead and push for better care from myself and the medical industry, and it's no longer what we just think is right, which is an attitude from previous eras," Mr Khazali explains.
"I think the next step could be an international technology, like an app, for patients and surgeons, that allows us to follow patients' journeys from diagnosis to years after treatment, to unlock some of the challenges we've been struggling with for a long time."

Mr Shaheen Khazali says the impact of endometriosis can be as devastating as cancer. Image credit: Shaheen Khazali
Mr Shaheen Khazali says the impact of endometriosis can be as devastating as cancer. Image credit: Shaheen Khazali
Mr Shaheen Khazali says an endometriosis patient once said they wished they had cancer and that it is a reflection on just how devastating the condition can be.
Mr Shaheen Khazali says an endometriosis patient once said they wished they had cancer and that it is a reflection on just how devastating the condition can be.
Recent Parliament debates on endometriosis has highlighted the need for further funding and research to understand the condition more.
Chloe, Shannon, Danni and Lisa hope that this reality changes for women so no girl is embarrassed by her period in school, no woman is overlooked in the workplace, and no woman feels pressurised to have children without the knowledge of her options.